How Shield Immunity Can Reduce Pandemic Intensity
Mitigation (e.g. mask wearing) and suppression (e.g. lockdowns) have emerged as the primary strategies to control and contain the spread of Covid-19. Both strategies focus on reducing the number of new infections by minimizing contact between potentially infected and susceptible individuals. Yet, these tactics raise questions of sustainability as long-term strategies given social and economic consequences.
Most interventions focus on the reduction of new viral transmission by reducing contact with others, but don't account for contact with individuals who have already been sick and recovered. Shield immunity leverages previously infected individuals at critical contact points. It is based on the assumption that recovered individuals (and/or individuals who have been vaccinated) have immunity and are protected from re-infection that could lead to transmission. Now, with increased vaccine distribution, there is a chance to leverage population-wide immunity to reduce onward transmission.
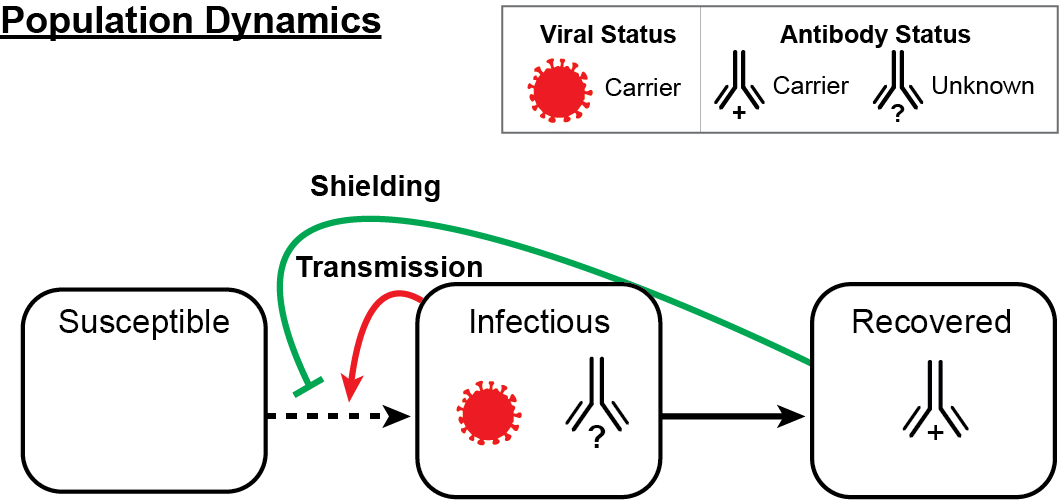
Population dynamics: In a population of susceptible, infectious, and recovered individuals, we can decrease the spread of infection by reducing contact between infectious and susceptible individuals with interaction substitution. With this method, interactions between potentially infectious individuals are replaced with recovered/antibody positive individuals at critical contact points (e.g., an antibody positive healthcare worker would interact with infectious patients as opposed to a susceptible healthcare worker). Black arrows denote flow of infection status. Red arrow signifies viral transmission and green line denotes protection (shielding) from transmission by an intervention using a recovered individual.
In a 2020 Nature Medicine paper, the Weitz group led efforts to develop an epidemiological intervention model that leverages serological tests to identify and deploy recovered individuals who have developed protective antibodies to SARS-CoV-2. In this model, antibody-positive individuals serve as focal points for sustaining safer interactions via interaction substitution. The objective of this intervention is to develop sufficient 'shield immunity' at the population scale to reduce epidemic intensity. Shield immunity works by increasing interactions with recovered individuals relative to individuals of unknown or susceptible status. Shield immunity can be utilized with social distancing measures, potentially enabling the same levels of infection reduction at the population scale with reduced economic and social costs of social distancing.
Despite the promise of shield immunity, there is a practical concern. How robust is the approach to variation in the specificity and sensitivity of antibody tests? In an ongoing collaboration, the Weitz and Lopman groups have evaluated the impact of the specificity and test capacity on both the reduction in disease transmission and the increase in the number of individuals who can safely return to work. As we show, highly specific tests (e.g., with upwards of 99% specificity) can reduce transmission while increasing the extent to which test status can help inform safer return to work policies. More information is available on our preprint.
We are currently working on new approaches to adapt shield immunity to healthcare settings. The key idea is to leverage serological tests and/or vaccinations to develop data- and epidemic-driven restaffing models to reduce risk of infection. Check back soon for more details.
While there are significant challenges to developing and implementing interventions that aim to build population-scale shield immunity, the magnitude of the current public health and economic crisis demands action, including new approaches to reopen schools and businesses. Our collaborative team continues to explore ways to assess the feasibility of shield immunity where recovered individuals may play a critical, active role in reducing the risk for others, alongside other measures including masks, social distancing, and test/tracing initiatives.